Research
 Our group aims to translate basic scientific advances into improved clinical management of cancer. We work in three main areas:
Our group aims to translate basic scientific advances into improved clinical management of cancer. We work in three main areas:
- Mechanisms of cervical neoplastic progression.
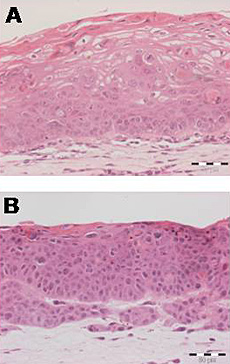
We study early events in the development of cervical carcinoma, in order to: (i) improve identification of the pre-cancers and early cancers that are more likely to progress; (ii) understand the effects and risks of treatments currently in use or development; (iii) identify new therapeutic strategies, targeting high-risk human papillomavirus (HR-HPV) oncogenes or host factors. We use an extensive archive of frozen and fixed cervical tissue, together with the unique W12 system, which represents an accurate and validated in vitro longitudinal model of cervical carcinogenesis. Questions of current interest are:
- Do specific genetic and/or epigenetic abnormalities underlie deregulation of HR-HPV oncogene expression during cervical neoplastic progression?
- Does the contribution of steroid hormones to cervical carcinogenesis depend on HR-HPV physical state and/or integration site?
- Does HR-HPV down-regulate cellular anti-virus receptors to promote persistence?
- Does HR-HPV-induced insertional mutagenesis contribute to clonal selection during neoplastic progression?
- Therapeutic targets in squamous cell carcinoma
Copy number gain of chromosome 5p is one of the most common genomic imbalances in cervical SCC. We discovered the role of two genes on chromosome 5p that are frequently over-expressed in advanced disease. The first is Drosha, a key enzyme in the microRNA biogenesis pathway, while the second is the cell surface cytokine receptor oncostatin M receptor (OSMR), which strongly predicts adverse overall survival in cervical SCC. OSMR is a promising target for antibody-mediated inhibition in SCC, a strategy that has had a major impact on HER2-positive breast cancers. Work in the lab currently focuses on targeting over-expressed OSMR to improve the treatment of advanced SCC. Questions of interest are:
- Is OSMR a prognostic marker and therapeutic target in SCCs of other anatomical sites?
- What are the consequences of OSMR over-expression in SCCs? What is the role of OSMR in constitutive activation of downstream signalling pathways?
- What is the effect of OSMR over-expression on the tumour microenvironment?
- Can therapeutic approaches for inhibiting OSMR signalling inhibit SCC progression, through reduced cell migration, invasion and angiogenesis?
- Malignant germ cell tumours and paediatric cancers
We study genetic changes in solid tumours of childhood, with a particular focus on malignant germ cell tumours (GCTs). Our paediatric GCT project is a national translational study, approved by the UK Children’s Cancer and Leukaemia Group (CCLG) and led by Professor Nick Coleman, Dr Matt Murray and Dr James Nicholson. We undertook detailed genomic and transcriptomic analyses of GCTs and were the first to identify important universal abnormalities in these tumours. In particular, we showed that microRNAs from the miR-371~373 and miR-302/367 clusters are highly over-expressed in all malignant GCTs, regardless of patient age, histological subtype or anatomical site. We are now extending this work as follows:
- Novel blood tests for paediatric cancer
We demonstrated that serum levels of miR-371~373 and miR-302/367 microRNAs are elevated at the time of malignant GCT diagnosis and may be tracked during treatment. We extended this work to show that a wide range of common solid tumours of childhood have specific diagnostic serum microRNA profiles. We are currently developing clinical protocols for serum microRNA testing in childhood cancer diagnosis, prognostication and monitoring. - Mechanisms of malignant GCT progression
We are studying the upstream causes of altered expression of non-coding RNAs in GCTs, together with the downstream consequences for driving malignant GCT progression
- Novel blood tests for paediatric cancer
- Matthew Murray, Academic Paediatric Oncologist Consultant
- Cinzia Scarpini, Senior Research Associate
- Ian Groves, Research Associate
- Emma Bell, Research Associate
- Dawn Ward, Senior Research Laboratory Technician
- Danita Pearson, Chief Research Laboratory Technician
- Katie Raby, Research Laboratory Technician
- Justyna Kucia, PhD student
- Emma Knight, PhD student
- Valtteri Tulkki, PhD student
- Shivani Bailey, PhD student
- Marta Ferraresso, PhD student
Recently left:
- Maria Munoz-Caffarel, Research Associate.
Email: mm794@cam.ac.uk (email active until June 2015)
Publications
Mechanisms of cervical neoplastic progression
1. Groves IJ and Coleman N (2015)
Invited review: Pathogenesis of human papillomavirus-associated mucosal disease.
The Journal of Pathology DOI: 10.1002/path.4496
2. Scarpini CG, Groves IJ, Pett MR, Ward D, Coleman N (2014)
Virus transcript levels and cell growth rates after naturally-occurring HPV16 integration events in basal cervical keratinocytes.
The Journal of Pathology 233:281-93
3. Hanning JE, Saini HK, Murray MJ, Caffarel MM, van Dongen S, Ward D, Barker EM, Scarpini CG, Groves IJ, Stanley MA, Enright AJ, Pett MR, Coleman N (2013)
Depletion of HPV16 early genes induces autophagy and senescence in a cervical carcinogenesis model, regardless of viral physical state.
The Journal of Pathology 231:354-66
4. Gray E, Pett MR, Ward D, Winder DM, Stanley MA, Roberts I, Scarpini CG, Coleman N (2010)
In vitro progression of human papillomavirus 16 episome-associated cervical neoplasia demonstrates fundamental similarities to integrant-associated carcinogenesis.
Cancer Research 70:4081-91
5. Dall KL, Scarpini CG, Roberts I, Winder DM, Stanley MA, Muralidhar B, Herdman MT, Pett MR, Coleman N (2008)
Characterisation of naturally occurring HPV16 integration sites isolated from cervical keratinocytes under non-competitive conditions.
Cancer Research 68:8249-59
6. Pett M, Coleman N (2007)
Integration of high-risk human papillomavirus: a key event in cervical carcinogenesis?
The Journal of Pathology 212:356-67
7. Pett MR, Herdman MT, Palmer RD, Yeo GS, Shivji MK, Stanley MA, Coleman N (2006)
Selection of cervical keratinocytes containing integrated HPV16 associates with episome loss and an endogenous antiviral response.
Proceedings of the National Academy of Sciences USA 103:3822-27
8. Herdman MT, Pett MR, Roberts I, Alazawi WO, Teschendorff AE, Zhang XY, Stanley MA, Coleman N (2006)
Interferon-beta treatment of cervical keratinocytes naturally infected with human papillomavirus 16 episomes promotes rapid reduction in episome numbers and emergence of latent integrants.
Carcinogenesis 27:2341-53.
Therapeutic targets in squamous cell carcinoma
9. Caffarel MM, Coleman N (2014)
Invited perspective: Oncostatin M receptor is a novel therapeutic target in cervical squamous cell carcinoma.
The Journal of Pathology 232:386-90
10. Caffarel MM, Chattopadhyay A, Araujo AM, Bauer J, Scarpini CG, Coleman N (2013)
Tissue transglutaminase mediates the pro-malignant effects of oncostatin M receptor over-expression in cervical squamous cell carcinoma.
The Journal of Pathology 231:168-79
11. Winder DM, Muralidhar B, English W, Ng G, Roberts I, Murray MJ, Pett MR, Murphy G, Coleman N (2011)
Overexpression of the oncostatin M receptor in cervical squamous cell carcinoma cells is associated with a pro-angiogenic phenotype and increased cell motility and invasiveness.
The Journal of Pathology 225:448-62
12. Muralidhar B, Winder DM, Palmer RD, Barbosa-Morais NL, Ng G, Mukherjee G, Roberts I, Murray MJ, Pett MR, Coleman N (2011)
Functional evidence that Drosha over-expression in cervical squamous cell carcinoma affects cell phenotype and microRNA profiles.
The Journal of Pathology 224:496-507
13. Ng G, Winder D, Muralidhar B, Gooding E, Roberts I, Pett M, Mukherjee G, Huang J, Coleman N (2007)
Gain and overexpression of the oncostatin M receptor occur frequently in cervical squamous cell carcinoma and are associated with adverse clinical outcome.
The Journal of Pathology 212:325-34
14. Muralidhar B, Goldstein LD, Ng G, Winder DM, Palmer RD, Gooding EL, Barbosa-Morais NL, Mukherjee G, Thorne NP, Roberts I, Pett MR, Coleman N (2007)
Global microRNA profiles in cervical squamous cell carcinoma depend on Drosha expression levels.
The Journal of Pathology 212:368-77
Malignant germ cell tumours and paediatric cancers
15. Murray MJ, Raby KL, Saini HK, Bailey S, Wool SV, Tunnacliffe JM, Enright AJ, Nicholson JC, Coleman N
Solid tumors of childhood display specific serum microRNA profiles. (2015)
Cancer Epidemiol Biomarkers Prev cebp.0669.2014. [Epub ahead of print]
16. Murray MJ, Saini HK, Siegler CA, Hanning JE, Barker EM, van Dongen S, Ward DM, Raby KL, Groves IJ, Scarpini CG, Pett MR, Thornton CM, Enright AJ, Nicholson JC, Coleman N (2013)
LIN28 expression in malignant germ cell tumors downregulates let-7 and increases oncogene levels.
Cancer Research 73:4872-84
17. Murray MJ, Coleman N (2012)
Testicular cancer: a new generation of biomarkers for malignant germ cell tumours.
Nature Reviews Urology 9:298-300
18. Palmer RD, Murray MJ, Saini HK, van Dongen S, Abreu-Goodger C, Muralidhar B, Pett MR, Thornton CM, Nicholson JC, Enright AJ, Coleman N (2010)
Malignant germ cell tumors display common microRNA profiles resulting in global changes in expression of mRNA targets.
Cancer Research 70:2911-23
19. Murray MJ, Saini HK, van Dongen S, Abreu-Goodger C, Palmer RD, Muralidhar B, Pett MR, Piipari M, Thornton CM, Nicholson JC, Enright AJ, Coleman N (2010)
The two most common histological subtypes of malignant germ cell tumour are distinguished by global microRNA profiles, associated with differential transcription factor expression.
Molecular Cancer 9:290
20. Palmer RD, Barbosa-Morais NL, Gooding EL, Muralidhar B, Thornton CM, Pett MR, Roberts I, Schneider DT, Thorne N, Tavaré S, Nicholson JC, Coleman N; Children's Cancer and Leukaemia Group. (2008)
Pediatric malignant germ cell tumors show characteristic transcriptome profiles.
Cancer Research 68:4239-47