Human cytomegalovirus (HCMV) infects the majority of people worldwide. After primary infection, the virus persists for the lifetime of the host at least in part by the ability of the virus to establish a ‘latent’ infection where it can infect undifferentiated cells, such as myeloid precursors, without the production of infectious virions.
Following the differentiation of these cells into terminally differentiated cells the virus can reactivate. In immune-competent individuals these reactivation events are quickly controlled by the immune system. However, in immune-compromised individuals (such as neonates and transplant patients) the virus can cause significant disease, long-term disabilities or death. Whilst there are antivirals they are not licensed for in utero treatment and are associated with poor bioavailability and high toxicity meaning that they are unsuitable for many patients. They also all target the late stages of the virus lifecycle and therefore lead to antiviral resistance.
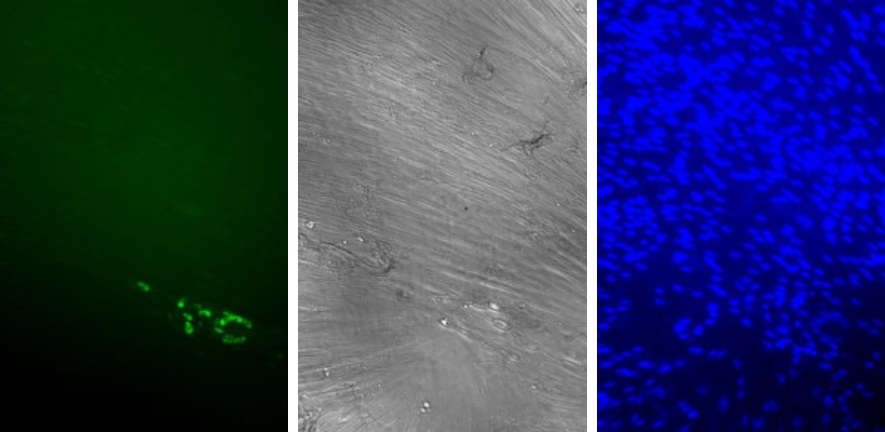
In our group, we are researching the molecular mechanisms that control HCMV latency. We have an established latency model system which has allowed us to interrogate many of the cellular and viral changes which occur within the latently infected cell using both screens and analysis of targeted individual molecular changes (with John Sinclair and Mark Wills, Department of Medicine, University of Cambridge, Matthew Reeves, UCL and Maria Carlan da Silva, Sao Paulo University).
These types of analyses have allowed the development of potential novel therapeutics. We have explored ‘kick and kill’ therapeutics as well as therapeutics which target specific viral proteins (with John Sinclair Mark Wills and Thomas Kledal at Synklino, Denmark, Sarah Hosgood and Michael Nicolson, Department of Surgery, Cambridge University and Bernard Kelly and Stephen Graham, Department of Pathology, University of Cambridge). We are also investigating the possibility of a ‘lock and block’ therapeutic approach to prevent virus reactivation in collaboration with Michael Nevels at the University of St Andrew’s . These would likely be used for transplant patients, perhaps treating the transplant material before transplant into the recipient. We are also interested in understanding how HCMV infects the placenta and the foetus and we are studying this in collaboration with Naomi McGovern in the Department of Pathology.
Current members of the group (full and part time):
Paula Rayner
Ryan Hall
Erica Appiah
Isabel Marchand Casas
Samuel Moulding
Publications:
‘Virus-Specific Nanobody-Chimeras Degrade the Human Cytomegalovirus US28 Protein in CD34+ Cells.’ Emma Poole *, Janika Schmitt, Stephen Graham, Bernard Kelly, John Sinclair. (2024) Sep 24;13(10):821. doi: 10.3390/pathogens13100821
‘The triterpernoid Momordin-Ic inhibits HCMV by preventing initiation of gene expression in eukaryotic cells’ Eleanor Bradley, Emma L. Poole, and Matthew B. Reeves Pathogens (2024) 13, x. Pathogens (2024) Jun 28;13(7):546. doi: 10.3390/pathogens13070546
‘SARS-CoV-2 ORF8 as a modulator of cytokine induction: Evidence and search for molecular mechanisms.’ Marília Inês Móvio2, Giovana Carneiro1, Isabella Lopes Martines1, Gilmara Barros de Lima1, Sergio Daishi Sasaki1, Alexandre Hiroaki Kihara2, Emma Poole3, Michael Nevels4, Maria Cristina Carlan da Silva. Viruses (2024), 16(1), 161;. https://doi.org/10.3390/v16010161
‘Repurposing an endogenous degradation domain for antibody-mediated disposal of cell-surface proteins’ Janika Schmitt, Emma Poole, Ian Groves, David J Owen, Stephen C Graham, John Sinclair, Bernard T Kelly. EMBO Rep (2024) doi: 10.1038/s44319-024-00063-3
‘MORC3 represses the HCMV major immediate early promoter in myeloid cells in the absence of PML nuclear bodies’Anna Champion, Alexandra Rowland, Levia Yee, Dick van den Boomen, Matthew Reeves, Paul Lehner, John Sinclair, Emma Poole Journal of Medical Virology (2023) https://doi.org/10.1002/jmv.29227
‘The Human Cytomegalovirus Latency-Associated Gene Product Latency UniqueNatural Antigen Regulates Latent Gene Expression’. Poole, E.; Lau, J.; Groves, I.;Roche, K.; Murphy, E.;Carlan da Silva, M.; Reeves, M.;Sinclair, J. Viruses (2023),15,1875. https://doi.org/10.3390/v15091875
Dr Emma Poole
Principle Investigator


