Submitted by Livia Harriman on Fri, 04/07/2025 - 10:20
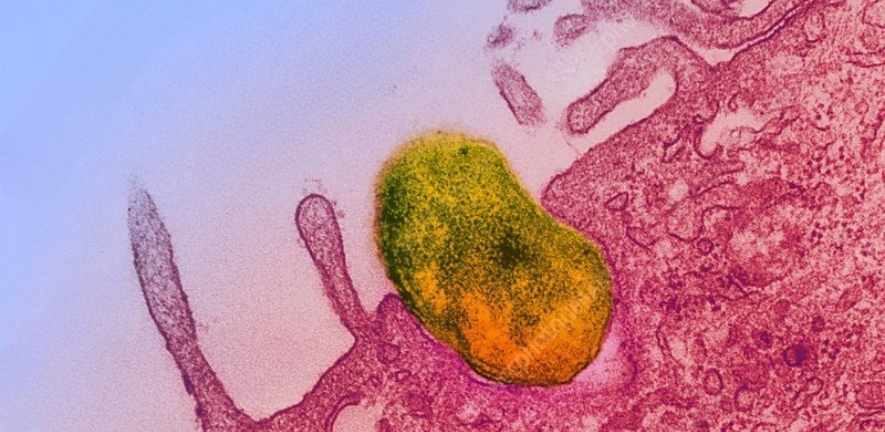
Scrub typhus, a severe and often life-threatening disease transmitted by mites, is caused by the intracellular bacterium Orientia tsutsugamushi. It's a major public health concern in parts of Asia, but despite its significance, the science behind why some strains cause deadly infections while others don’t has remained murky—until now.
A new study published by Jeanne Salje in PLOS Pathogens takes a significant step forward in decoding this puzzle. By comparing the virulence of seven genetically diverse strains of O. tsutsugamushi, the team discovered that the bacterium's ability to cause disease stems not from a single "smoking gun" gene, but rather a complex web of genetic and host immune interactions.
Not Just One Villain: The Many Faces of O. tsutsugamushi
The research team utilised a mouse model to investigate the impact of each of the seven strains on weight loss, survival, bacterial load, and immune response. The most virulent strains—Kato and Ikeda—triggered severe illness and high cytokine levels, mirroring patterns seen in the most dangerous human infections.
In contrast, the strain TA686 didn’t cause illness in mice and hasn’t been linked to human disease, marking it as avirulent. This strain also showed a unique behaviour inside host cells, localising differently and expressing higher levels of a surface protein called ScaC.
No One Gene to Rule Them All
One of the most surprising findings? There is no single gene or growth pattern that predicts the danger of a strain. While some genes were uniquely present in the most virulent strains, and others were absent in the avirulent ones, these alone couldn't explain the whole picture. Instead, the study suggests that virulence is distributed across the genome, with dozens of effector proteins interacting in complex, unpredictable ways.
The Host Fights Back—But At a Cost
The researchers also explored how each strain triggered immune responses in mice. The more virulent the strain, the higher the levels of inflammatory cytokines, such as IL-6, IL-10, IFN-γ, and MCP-1. These same molecules are also found in high levels in severely ill human patients, reinforcing the connection between strain-specific responses and clinical severity.
Why This Matters
This study doesn't just help explain the biology of scrub typhus—it’s a step toward better diagnostics and vaccines. Understanding that virulence is multifactorial means that future treatments must take into account strain diversity. It also emphasises the importance of studying multiple strains rather than relying on a few long-used laboratory isolates.
What’s Next?
The team calls for expanded research on O. tsutsugamushi strains—especially those not yet detected in human cases. There may be entire populations of avirulent strains circulating in mite reservoirs, escaping current surveillance.
As sequencing technologies improve and more comprehensive models are developed, scientists are moving closer to a full understanding of this complex pathogen. Until then, this study is a powerful reminder that in the microbial world, disease severity is often the result of many subtle, interacting factors.
Read the full paper here: PLOS Pathogens, June 2025

