Dr Peter Bull and colleagues publish new research in the journal Nature
Malaria still claims over 400,000 lives every year, mostly due to infection by a single species of malaria parasite Plasmodium falciparum. However, people living in the presence of regular exposure to malaria parasite infection develop naturally acquired immunity that protects them during their adult lives. One route to finding new vaccines against malaria is by identifying the molecular targets of this natural protective immune response.
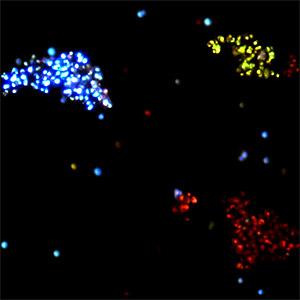
Severe, life-threatening malaria occurs during a stage in Plasmodium falciparum parasite life-cycle when these parasites infect and hide within red blood cells. Several previous studies suggest that a major component of the protective immune response is directed towards highly variable parasite molecules called “variant surface antigens” that are inserted by parasites into the surface of infected red blood cells. These molecules are used by parasites to manipulate the infected cells so that they stick to the linings of blood vessels that supply organs in the body including the brain. It is the accumulation of large numbers of parasite-infected red blood cells in the brain that causes life-threatening malarial coma known as “cerebral” malaria.
Several molecular “families” of variant surface antigens are manufactured by Plasmodium falciparum. These include PfEMP1, RIFINs and STEVOR. Much previous emphasis has been placed on the most prominent of these, PfEMP1, but recent reports also support an important role for RIFINs and STEVOR.
Despite the key role that variants surface antigens play both as targets of naturally acquired immunity and in the pathology of severe malaria they are often regarded as unsuitable vaccine candidates because of their high level of molecular diversity. Finding antibodies that cross react with a broad range of Plasmodium falciparum variant surface antigens from different individuals would potentially lead to the development of new interventions against malaria.
A study reported online in the journal Nature has identified two rare individuals who may provide information for the development of such interventions. Surprisingly, these two individuals carried antibodies that recognize, not the most prominent molecules PfEMP1, but RIFINs. At the molecular level, this reactivity in the antibodies was brought about through independent and novel events that occurred during their natural generation in the body, in which migration and insertion of DNA occurred from a non-antibody gene called LAIR1. The authors suggest that finding the molecular shape that these antibodies recognize on RIFINs may lead to a potential vaccine. However, they still do not know whether such antibodies, when present, would be sufficient to protect individuals from life threatening malaria or how commonly natural LAIR1 insertions occur in other antibodies.