Patients who are admitted to intensive care are at high risk of complications from infection, both as the presenting pathology and developing as complications during their admission. Pneumonia, a severe infection of the alveolar airspace, is both the commonest infective reason for admission and the commonest secondary infection acquired in the ICU.
Dr Conway Morris has demonstrated that patients in intensive care have impaired immune function, and has identified several defects in neutrophil anti-microbial functions. These dysfunctions occur before patients develop secondary infections, and predict the risk of acquiring one. This holds the promise of being able to prevent secondary infections by targeting immune dysfunction in at-risk patients.
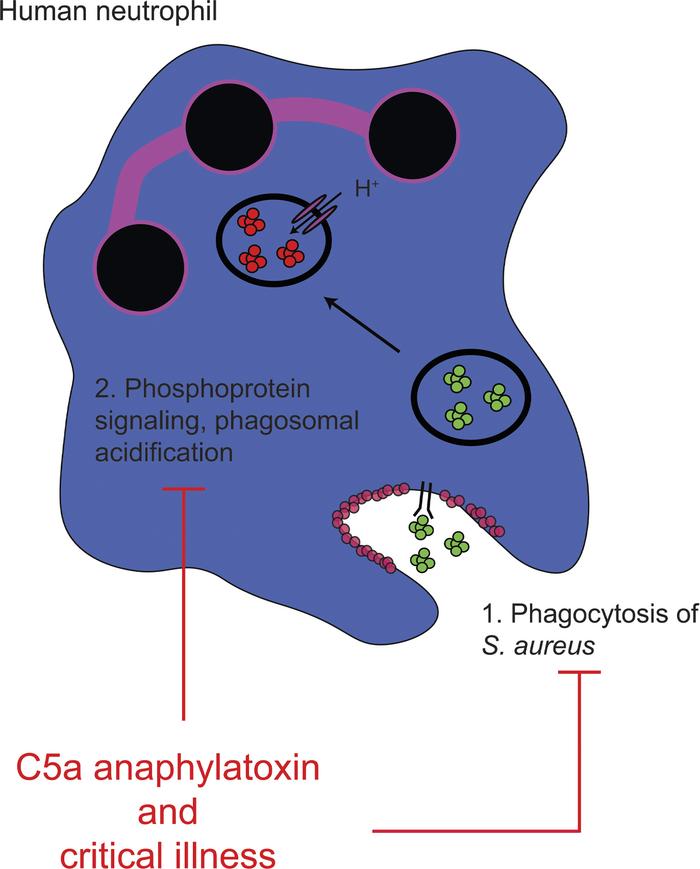
One of the predominant drivers of this dysfunction is the pro-inflammatory molecule C5a, a component of the complement cascade which is released in high concentrations in critically ill patients. Dr Conway Morris demonstrated how C5a can drive impaired phagocytosis via phosphoinositide-3-kinase delta, and that this defect can be reversed using granulocyte-macrophage colony stimulating factor, which has led to a recent phase II clinical trial. Using a phosphoproteomic technique developed in his lab, he has recently identified further defects in phagosomal maturation induced by C5a. His current work focuses on understanding the signalling pathways which are activated when the neutrophil encounters a bacterial pathogen, how these are influenced by the inflammatory environment the cells are in and how this impairs antimicrobial responses.
Biography
Andrew is a practicing intensive care physician and clinician scientist whose research focuses on severe infections in intensive care patients. He is interested in how the immune system fails in critical illness and how this leads to infections, most especially pneumonia.
His undertook degrees in medicine and biomedical science at the University of Glasgow before moving to Edinburgh where he completed a PhD in critical care immunology, identifying the complement component C5a as a key mediator in neutrophil dysfunction in critically ill patients. After a period as a Clinical Lecturer in Intensive Care Medicine at the University of Edinburgh he moved to Cambridge to take up an NIHR Academic Clinical Lectureship, followed by a Wellcome Trust Clinical Research Career Development Fellowship. He is currently an MRC Clinician Scientist in the Department of Medicine and Visiting Scientist in the Department of Pathology, where he works closely with Klaus Okkenhaug’s group in a shared lab space. His group in the Department of Pathology seeks to understand the signalling pathways that underpin the neutrophil response to pathogens, and how these are disrupted in critical illness and sepsis.
Research
Research Interests
Neutrophil biology
Host-microbe interactions
Critical illness and Sepsis
Pneumonia
Publications
Wood AJ, Vasallo AM, Ruchaud-Sparagano MH, Scott J, Zinatto C, Gonzalez-Tejedo C, Kamal K, D’Santos C, Simpson AJ, Menon DK, Summers C, Chilvers ER, Okkenhaug K, Conway Morris A (Corresponding author). C5a modulates neutrophil phosphoproteomic remodelling during phagocytosis, impairing phagosomal maturation. JCI Insight2020;5(15):137029. 10.1172/jci.insight.137029
Conway Morris A (Corresponding author), Datta D, Shankar-Hari M, Stephen J, Weir CJ, Rennie J, Antonelli J, Bateman A, Warner N, Judge K, Keenan J, Wang A, Burpee T, Brown KA, Lewis SM, Mare T, Roy AI, Hulme G, Dimmick I, Rossi AG, Simpson AJ, Walsh TS. Cell surface signatures of immune dysfunction risk stratify critically ill patients: INFECT Study. Intensive Care Med. 2018;44:627-635 10.1007/s00134-018-5247-0
Pinder EM, Rostron AJ, Hellyer TP, Ruchaud-Sparagano MH, Scott J, Macfarlane JG, Wiscombe S, Widdrington JD, Roy AI, Linnett VC, Baudouin SV, Wright SE, Chadwick T, Fouweather T, Juss JK, Chilvers ER, Bowett SA, Parker J, McAuley DF, Conway Morris A, Simpson AJ. Randomised controlled trial of GM-CSF in critically ill patients with impaired neutrophil phagocytosis. Thorax.2018;73:918-925 10.1136/thoraxjnl-2017-211323
TJ Nolan, NJ Gadsby, Hellyer TP ,Templeton KE, McMullan R , McKenna JP, Rennie J, Robb CT, Walsh TS, Rossi AG, Conway Morris A (Joint Senior and Corresponding author), Simpson AJ+. Low-pathogenicity Mycoplasma species alter human monocyte and macrophage function and are highly prevalent amongst patients with ventilator-acquired pneumonia. Thorax, 2016 Jul;71(7):594-600. 10.1136/thoraxjnl-2015-208050
Conway Morris A (corresponding author), Anderson N, Brittan M, Wilkinson TS, McAuley DF, Antonelli J, McCulloch C, Barr LC, Dhaliwal K, Jones RO, Haslett C, Hay AW, Swann DG, Laurenson IF, Davidson DJ, Rossi AG, Walsh TS, Simpson AJ. Combined dysfunctions of immune cells predict nosocomial infection in critically ill patients. Br J Anaesth, 2013 Nov;111(5):778-87. 10.1093/bja/aet205
Conway Morris A (Corresponding author), Brittan M, Wilkinson TS, McAuley DF, Antonelli J, McCulloch C, Barr LC, McDonald NA, Dhaliwal K, Jones RO, Mackellar A, Haslett C, Hay AW, Swann DG, Anderson N, Laurenson IF, Davidson DJ, Rossi AG, Walsh TS, Simpson AJ. C5a-mediated neutrophil phagocytic dysfunction is RhoA-dependent and predicts nosocomial infection in critically ill patients. Blood. 2011;117:5178-88. 10.1182/blood-2010-08-304667
Conway Morris A (Corresponding author), Kefala K, Wilkinson TS, Dhaliwal K, Farrell L, Walsh T, Mackenzie SJ, Reid H, Davidson DJ, Haslett C, Rossi AG, Sallenave JM, Simpson AJ. C5a mediates peripheral blood neutrophil dysfunction in critically ill patients. Am J Respir Crit Care Med. 2009;180:19-28. 10.1164/rccm.200812-1928OC
Neutrophils in critical illness
Finlay LD, Conway Morris A, Deane AM, Wood AJ. Neutrophil kinetics and function after major trauma: A systematic review. World J Critical Care Medicine 10, 260–277 (2021)
Scott J, Ruchaud-Sparagano MH, Musgrave K, Roy AI, Wright SE, Perry JD, Conway Morris A, Rostron AJ, Simpson AJ. Phosphoinositide 3-kinase delta inhibition improves neutrophil bacterial killing in critically ill patients at high risk of infection. J Immunol. 2021 Oct 1;207(7):1776-1784. doi: 10.4049/jimmunol.2000603. Epub 2021 Sep 8
Bashant KR, Aponte AM, Randazzo D, Sangsari PR, Wood AJT, Bibby JA, West EE, Vassallo A, Manna Z, Playford MP, Jordan N, Hasni S, Gucek M, Kemper C, Conway Morris A, Morgan NY, Toepfner N, Guck J, Mehta NN, Chilvers ER, Summers C, Kaplan MJ. Proteomic, biomechanical, and functional analyses define neutrophil heterogeneity in systemic lupus erythematosus. Ann Rheum Dis. 2021 Feb;80(2):209-218.
Evans SJ, Roberts AEL, Conway Morris A, Simpson AJ, Harris LG, Mack D, Jenkins RE, Wilkinson TS. Contrasting effects of linezolid on healthy and dysfunctional human neutrophils: reducing C5a-induced injury. Sci Rep. 2020;10:16377
Shankar-Hari M, Datta D, Wilson J, Assi V, Stephen J, Weir CJ, Rennie J, Antonelli J, Bateman A, Felton J, Warner N, Judge K, Keenan J, Wang A, Burpee A, Brown AK, Lewis SM, Mare T, Roy AI, Wright J, Hulme G, Dimmick I, Gray A, Rossi AG, A Simpson J, Conway Morris A, Walsh TS. Early PREdiction of Sepsis using leukocyte surface biomarkers: The ExPRES-Sepsis cohort study. Intensive Care Med. 2018;315:801-13
Wood AJ, Vassallo A, Summers C, Chilvers C, Conway Morris A. C5a anaphylatoxin and its role in critical illness-induced organ dysfunction. Eur J Clin Invest. 2018;48(12):e13028
Conway Morris A, Wilson J, Shankar-Hari M. Immune activation in sepsis. Critical Care Clinics. 2018;34:29-42.
Dorward D, Lucas CD, Doherty MK, Chapman GB, Scholefield E, Conway Morris A, Felton JM, Kipari T, Humphries D, Robb CT, Simpson AJ, Whitfield P, Haslet C, Dhaliwal K, Rossi AG. Novel role for endogenous mitochondrial formylated peptide-driven formyl peptide receptor 1 signaling in Acute Respiratory Distress Syndrome. Thorax. 2017;72:928-936.
Scott J, Harris GJ, Pinder EM, Macfarlane JG, Hellyer TP, Rostron AJ, Conway Morris A, Thickett DR, Perkins GD, McAuley DF,6, Widdrington JD, Wiscombe S, Baudouin SV, Roy AI, Linnett VC, Wright SE, Ruchaud-Sparagano MH, Simpson AJ. EPAC activation reverses neutrophil dysfunction induced by beta2-agonists, corticosteroids and critical illness. J Allergy Clin Immunol. 2016 Feb;137(2):535-44.
+ Wilkinson TS, +Conway Morris A, +Kefala K, O'Kane CM, Moore NR, Booth NA, McAuley DF, Dhaliwal K, Walsh TS, Haslett C, Sallenave JM, Simpson AJ. Ventilator-associated pneumonia is characterized by excessive release of neutrophil proteases in the lung. Chest, 2012;142:1425-32 (+ joint first authorship)
Diagnostics in pneumonia (inc. COVID-19)
Conway Morris A, Sharrocks K, Bousfield R, Kermack L, Maes M, Higginson E, Forrest S, Pereria-Dias J, Cormie C, Old T, Brooks S, Hamed I, Koenig A, Turner A, White P, Floto RA, Dougan G, Gkrania-Klotsas E, Gouliouris T, Baker S, Navapurkar V. The removal of airborne SARS-CoV-2 and other microbial bioaerosols by air filtration on COVID-19 surge units. MedRxiv 2021. doi:10.1101/2021.09.16.21263684
Navapurkar V, Bartholdson Scott J, Maes M , Higginson E, Forrest S, Pereira Dias J, Parmar S, Heasman-Hunt E, Polgarova P, Brown J, Titti L, Smith WPW, Routledge M, Sapsford D, Torok, E Enoch D, Wong V, Curran MD, Brown N, Herre J, Dougan G, Conway Morris A. Development and implementation of a customised rapid syndromic diagnostic test for severe pneumonia. MedRxiv 2020 https://doi.org/10.1101/2020.06.02.20118489
Lockhart SM, Griffiths H, Petrisor B, Usman A, Calvo‐Latorre J, Heales, L, Bansiya V, Mahroof R, Conway Morris A. (2021), The excess insulin requirement in severe COVID‐19 compared to non‐COVID‐19 viral pneumonitis is related to the severity of respiratory failure and pre‐existing diabetes. Endocrinol Diab Metab 2021 Feb 11;4(3):e00228
Maes M, Higginson E, Pereira-Dias J, Curran MD, Parmar S, Khokhar F, Cuchet-Lourenço D, Lux J, Sharma-Hajela S, Ravenhill B, Hamed I, Heales L, Mahroof R, Solderholm A, Forrest S, Sridhar S, Brown NM, Baker S, Navapurkar V, Dougan G, Bartholdson Scott J, Conway Morris A. Ventilator-associated pneumonia in critically ill patients with COVID-19. Crit Care. 2021 Jan 11;25(1):25.
Luyt CE, Bouadma L, Conway Morris A, Dhanani JA, Kollef M, Lipman J, Martin-Loeches I, Nseir S, Ranzani OT, Roquilly A, Schmidt M, Torres A, Timsit JF. Pulmonary infections complicating acute respiratory distress syndrome.Intensive Care Med. 2020 Dec;46(12):2168-2183.
Hamed I, Shaban N, Nassar M, Cayir D, Love S, Curran MD, Webb S, Yang H, Watson K, Rostron T, Navapurkar V, Mahroof R, Conway Morris A. Paired nasopharyngeal and deep lung testing for SARS-CoV2 reveals a viral gradient in critically ill patients: a multi-centre study. Chest. 2020 Oct 15:S0012-3692(20)34909-6. doi: 10.1016/j.chest.2020.10.017. Epub ahead of print.
Tong A, Elliott JH, Azevedo LC, Baumgart A, Bersten A , Cervantes L , Chew DP, Cho Y, Cooper T , Crowe S, Douglas IS, Evangelidis N, Flemyng E, Hannan, Horby P, Howell M , Lee J, Liu E, Lorca E, Lynch D, Marshall JC, Gonzalez MA, McKenzie A, Manera KE, McLeod C, Mehta S, Mer M , Conway Morris A, Nseir S, Povoa P, Reid M, Sakr Y, Shen N, Smyth AR, Snelling T , Strippoli GFM , Teixeira-Pinto A , Torres A, Turner T , Viecelli AK,Webb S, Williamson PR, Woc-Colburn L, Zhang J , Craig JC, COVID-19-Core Outcomes Set (COS) Workshop Investigators. Core Outcomes Set for Trials in People With Coronavirus Disease 2019. Crit Care Med. 2020 Nov;48(11):1622-1635.
Evangelidis N, Tong A, Howell M, Teixeira-Pinto A, Elliott JH, Azevedo LC, Bersten A, Cervantes L, Chew DP, Crowe S, Douglas IS, Flemyng E, Horby P, Lee J, Lorca E, Lynch D, Marshall JC, McKenzie A, Mehta S, Mer M, Conway Morris A, Nseir S, Povoa P, Reid M, Sakr Y, Shen N, Smyth AR, Snelling T, Strippoli GFM, Torres A, Turner T, Webb S, Williamson PR, Woc-Colburn L, Zhang J, Baumgart A, Cabrera S, Cho Y, Cooper T, Guha C, Liu E, Gonzalez AM, McLeod C, Natale P, Saglimbene V, Viecelli AK, Craig JC; COVID-19-Core Outcomes Set (COS) Survey Investigators.International Survey to Establish Prioritized Outcomes for Trials in People With Coronavirus Disease 2019 Crit Care Med. 2020 Nov;48(11):1612-1621
Loughlin L, Hellyer T, White PL, McAuley D, Conway Morris A, Posso R, Richardson M, Denning D, Simpson AJ, McMullan R. Pulmonary aspergillosis in patients with suspected ventilator-associated pneumonia in UK Intensive Care Units. Am J Respir Crit Care Med. 2020;10.1164.
Jones NK, Conway Morris A, Curran MD, et al. Evaluating the use of a 22-pathogen TaqMan array card for rapid diagnosis of respiratory pathogens in intensive care. J Med Microbiol. June 2020:p.7-p.8.
Tabah A, Ramanan M, Laupland KB, Buetti N, Cortegiani A, Mellinghoff J, Conway Morris A, Comporota A, Zappella N, Elhadi M, Povoa P, Amrein K, Vidal G, Derde L, Bassetti M, Francois G, Ssi yan kai N, De Waele JJ. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): An international survey J Crit Care. 2020;59:70-75
Arulkumaran N, Routledge M, Schlebusch S, Lipman J, Conway Morris A. Antimicrobial-associated harm in critical care: a narrative review. Intensive Care Medicine. 2020;46:225-235
Hellyer T, McAuley DF, Walsh TS, Anderson N, Conway Morris A, Singh S, Dark P, Roy AI, Perkins GD, McMullan R, Emerson LM, Blackwood B, Wright SE, Kefala K, O’Kane CM, Baudouin SV, Paterson RL, Rostron AJ, Agus A, Bannard-Smith J, Robin NM, Welters ID, Bassford C, Yates B, Spender C, Laha SK, Hulme J, Bonner S, Linnett V, Sonksen J, Van Den Broek T, Boschman G, Keenan J, Scott J, Allen AJ, Phair G, Parker J, Bowett SA, Simpson AJ. Randomised controlled trial and process evaluation of biomarker-guided antibiotic stewardship in suspected ventilator-associated pneumonia. Lancet Resp Med, 2020;8:182-191.
Rello J, Vandana KE, Lagunes L, Alves J, Wunderink RG; Conway Morris A, Nicolas J, Alp E, Zhang Z, and TOTEM Study contributors. Global Priority List of TOp TEn resistant Microorganisms at Intensive Care (TOTEM study): A prioritization exercise based on multi-criteria decision analysis. Eur J Clin Micro Infect Dis. 2019 Feb;38:319-323.
Conway Morris A. Management of pneumonia in ICU. J Emerg Crit Care Med. 2018:2;101.
Conway Morris A, Gadsby N, McKenna JP, Hellyer TP, Dark P, Singh S, Walsh TS, McAuley DF, Templeton K, SimpsonAJ, McMullan R. 16S pan-bacterial PCR can accurately identify patients with ventilator-acquired pneumonia. Thorax, 2017;72:1046-1048.
Gadsby NJ, Russell CD, McHugh MP, Mark M, Conway Morris A, Laurenson IF, Hill AT, Templeton KE Comprehensive molecular testing for respiratory pathogens in community-acquired pneumonia. Clin Infect Dis, 2016;62(7):817-23
Gadsby NJ, McHugh MP, Russell CD, Mark H, Conway Morris A, Laurenson IF, Hill AT, Templeton KE. Development of two real-time multiplex PCR assays for the detection and quantification of eight key bacterial pathogens in lower respiratory tract infection. Clin Microbiol Infect. 2015 Aug;21(8):788.e1-788.e13
Hellyer TP, Conway Morris A, McAuley DF, Walsh TS, Anderson NH, Singh S, Dark P, Roy AI, Baudouin S, Wright SE, Perkins GD, Kefala K, Jeffels M, McMullan R, O’kane C, Spencer C, Laha S, Robin N, Gossain S, Gould K, Ruchaud-Sparagno MH, Scott J, Browne EM, Macfarlane JG, Wiscombe S, Widdrington JD, Dimmick I, Laurenson IF, Nauwelaers F, Simpson AJ. Diagnostic accuracy of pulmonary host inflammatory mediators in the exclusion of ventilator-acquired pneumonia. Thorax.2015;70(1):41-7
Browne E, Hellyer TP, Baudouin SV, Conway Morris A, Linnett V, McAuley DF, Perkins GD, Simpson AJ. A national survey of the diagnosis and management of suspected ventilator-associated pneumonia. BMJ Open Respir Res. 2014 Dec 16;1(1):e000066.
Brittan M, Barr LC, Anderson N, Conway Morris A, Duffin R, Marwick JA, Rossi F, Johnson S, Dhaliwal K, Hirani N, Rossi AG, Simpson AJ Functional characterisation of human pulmonary monocyte-like cells in lipopolysaccharide-mediated acute lung inflammation. J Inflamm. 2014 Mar 31;11(1):9.
Ferguson GD, Gadsby NJ, Henderson SS, Hardie A, Kalima P, Conway Morris A, Hill AT, Cunningham S, Templeton KE. Clinical outcomes and macrolides resistance in mycoplasma pneumoniae infection in Scotland. J Med Microbiol. 2013;62(12):1876-82
Conway Morris A, Hay AW, Swann DG, Everingham K, McCulloch C, McNulty J, Brooks O, Laurenson IF, Cook B, Walsh TS. Reducing ventilator-associated pneumonia in Intensive Care: impact of implementing a care bundle. Crit Care Med. 2011;39:2218-24
Conway Morris A, Kefala K, Simpson AJ, Wilkinson TS, Everingham K, Kerslake D, Raby S, Laurenson IF, Swann DG, Walsh TS. Evaluation of diagnostic methodology on the reported incidence of ventilator-associated pneumonia. Thorax. 2009;64:516-522.
Conway Morris A, Kefala K, Wilkinson TS, Moncayo-Nieto OL, Dhaliwal K, Farrell L, Walsh TS, Mackenzie SJ, Swann DG, Andrews PJ, Anderson N, Govan JR, Laurenson IF, Reid H, Davidson DJ, Haslett C, Sallenave JM, Simpson AJ. Diagnostic importance of pulmonary interleukin-1 beta and interleukin-8 in ventilator-associated pneumonia. Thorax. 2010 65: 201-207
Miscellaneous
Zochios V, Singh Chandan J, Schulz MJ, Conway Morris A, Parhar KK, Gimenez-Mila M, Gerrard C, Vuylsteke A, Klein AA. The Effects of Escalation of Respiratory Support and Prolonged Invasive Ventilation on Outcomes of Cardiac Surgical Patients: A Retrospective Cohort Study. J Cardiothorac Vasc Anaes. 2019 Nov 8. pii: S1053-0770(19)31129-2.
Moncayo-Nieto OL, Wilkinson TS, Brittan M, McHugh BJ, Jones RO, Conway Morris A, Walker WS, Davidson DJand Simpson AJ. Differential response to bacteria, and TOLLIP expression, in the human respiratory tract. BMJ Open Resp Res 2014;1:e000046
Jones RO, Brittan M, Anderson NH, Conway Morris A, Murchison JT, Walker WS, John Simpson A. Serial characterisation of monocyte and neutrophil function after lung resection BMJ Open Resp Res 2014;1:1 e000045
Jiwaji Z, Nunn K, Conway Morris A, Wyncoll D, Simpson AJ, Rossi A, Walsh T. Leuco-depleted blood transfusion does not produce an inflammatory response in critically ill adults, results from a randomised controlled trial. Transfusion. 2014 Oct;54(10):2404-11.
Barr LC, Brittan M, Conway Morris A, McAuley DF, McCormack C, Fletcher AM, Richardson H, Connell M, Patel D, Wallace WA, Rossi AG, Davidson DJ, Manson L, Turner M, Hirani N, Walsh TS, Anderson NH, Dhaliwal K, Simpson AJ. An RCT of peripheral blood mononuclear cell depletion in experimental human lung inflammation. Am J Respir Crit Care Med. 2013;188:449-55.
Barr L, Brittan M, Conway Morris A, Stewart A, Dhaliwal K, Anderson N, Turner M, Manson L, Simpson AJ.Pulmonary and systemic effects of mononuclear leukapheresis. Vox Sang. 2012 Nov;103:275-83
Dhaliwal K, Scholefield E, Ferenbach D, Gibbons M, Duffin R, Dorward DA, Conway Morris A, Humphries D, MacKinnon A, Wilkinson TS, Wallace WA, van Rooijen N, Mack M, Rossi AG, Davidson DJ, Hirani N, Hughes J, Haslett C, Simpson AJ. Monocytes control second-phase neutrophil emigration in established LPS-induced murine lung injury. Am J Respir Crit Care Med. 2012;186:514-24
Brittan M, Barr L, Conway Morris A, Duffin R, Rossi F, Johnston S, Monro G, Anderson N, Rossi AG, McAuley DF, Haslett C, Hirani N, Dhaliwal K, Simpson AJ. A novel monocyte-like subpopulation in the human lung following LPS inhalation. European Resp Jnl. 2012 ;40:206-14
Conway Morris A, Forrest R, Campbell A. Thrombo-prophylaxis in intensive care: a nationwide, multi-disciplinary quality improvement project. J Intensive Care Soc. 2010;11:2-6
Lowder B, Guinane C, Ben Zakor N, Weinert L, Conway Morris A, Cartwright R, Simpson AJ, Rambaut A, Nubel U, Fitzgerald JR. Recent human to poultry host jump, adaptation, and pandemic spread of Staphylococcus aureus. PNAS. 2009 106:19545-19550
Conway Morris A, Howie N. Pain in medical patients: an under-recognised problem? J R Coll Physicians Edinb 2009; 39:292–5
Lyon R, Conway Morris A, Caesar D, Gray S, Gray A. Chest pain presenting to the emergency department: to risk stratify with GRACE or TIMI? Resuscitation 2007; 74 (1):90-93.
Conway Morris A, Caesar D, Gray S, Gray A. The TIMI risk score accurately risk stratifies patients with undifferentiated chest pain presenting to an Emergency Department. Heart 2006;92 (9):1333-1334.
Editorials, Book Chapters
Conway Morris A. New movement in sepsis immunotherapeutics; a role for prokineticin 2? Crit Care Med. In press
Velu PP, Lucas CD, Conway Morris A. Post-mortem dissection of COVID-19: a pathogenic role for macrophages? Intensive Care Med. 2021 Sep 1:1–4. doi: 10.1007/s00134-021-06509-9
Conway Morris A, Kohler K, Shankar-Hari M. ARDS sub-phenotypes - searching for Rorschach amongst the roentgenograms? Thorax. 2021 Jul 12:thoraxjnl-2021-217428. doi: 10.1136/thoraxjnl-2021-217428.
Conway Morris A. CAR-T cells: shock of the new. Crit Care Med. In press
Conway Morris A. VAP - quantum uncertainty in the ICU? Crit Care Med. 2018;46:1007-1008
Conway Morris A. Triage during pandemic influenza: seeking absolution in numbers? B J Anaes. 2015 Jun;114(6):865-7
Walsh TS, Conway Morris A, Simpson AJ. Ventilator Associated Pneumonia: can we ensure that a quality indicator does not become a game of chance? Br J Anaes. 2013;111:333-7.
Book chapters
Conway Morris A, Tong A. Novel treatments and trials in COVID-19. COVID-19 Pandemic. 2022;109-120. doi:10.1016/B978-0-323-82860-4.00006-9
Teaching and Supervisions
Part 1B Immunology
Group Members
Muhammad Iqbal
Dr Matthew Routledge
Available for supervision of PhD and MPhil students
Other Professional Activities
Deputy Chair of the Infection Section, European Society of Intensive Care Medicine


 https://orcid.org/0000-0002-3211-3216
https://orcid.org/0000-0002-3211-3216